EMR Development: Benefits and Challenges
- Updated: Nov 13, 2024
- 12 min
Is it profitable to launch a healthcare solution like EMR in 2025?
Well, in the post-COVID world, venture capitalists find it harder to get excited about investing in digital health.
PitchBook data shows that healthcare IT deal activity remained steady in the first quarter of 2025, with 74 deals amounting to approximately $1 billion.
This is 3% higher compared to the same period last year.
However, the situation is getting better now.
At the American Telemedicine Association’s Nexus conference, investors shared their insights on the market.
They highlighted that they have a cautious but positive outlook for early-stage and growth-stage investments.
Now, investors are looking for healthcare tech solutions with defined and proven clinical outcomes.
They also emphasized the importance of clear AI applications and the complexities of value-based care models (learn more about AI jargon in our AI glossary).
Overall, investors are ready to support high-quality healthcare startups that demonstrate measurable benefits.
In fact, with the integration of AI, the rise of wearable devices, the potential of 5G, and insights from big data, the future of the EHR and EMR software industry looks very promising.
In this article, we’ll explore the benefits and challenges of EHR software development as well as how to build your own EMR.
Unlock your startup potential now — start transforming your vision into a scalable solution with our expert developers today!
What is an Electronic Medical Record (EMR)?
An electronic medical record (EMR) is a digital collection of medical information about a patient stored on a computer.
This medical information is spread across different healthcare settings.
It may include such clinical data as demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics, and billing information. Here is more about how radiology information systems work and integrate with other systems.
These systems are becoming popular, and market research is only proving this point.
The U.S. Electronic Medical Records (EMR) Market was valued at $5.92 billion in 2023 and is expected to reach $8.10 billion by 2029, growing at a CAGR of 5.36%. 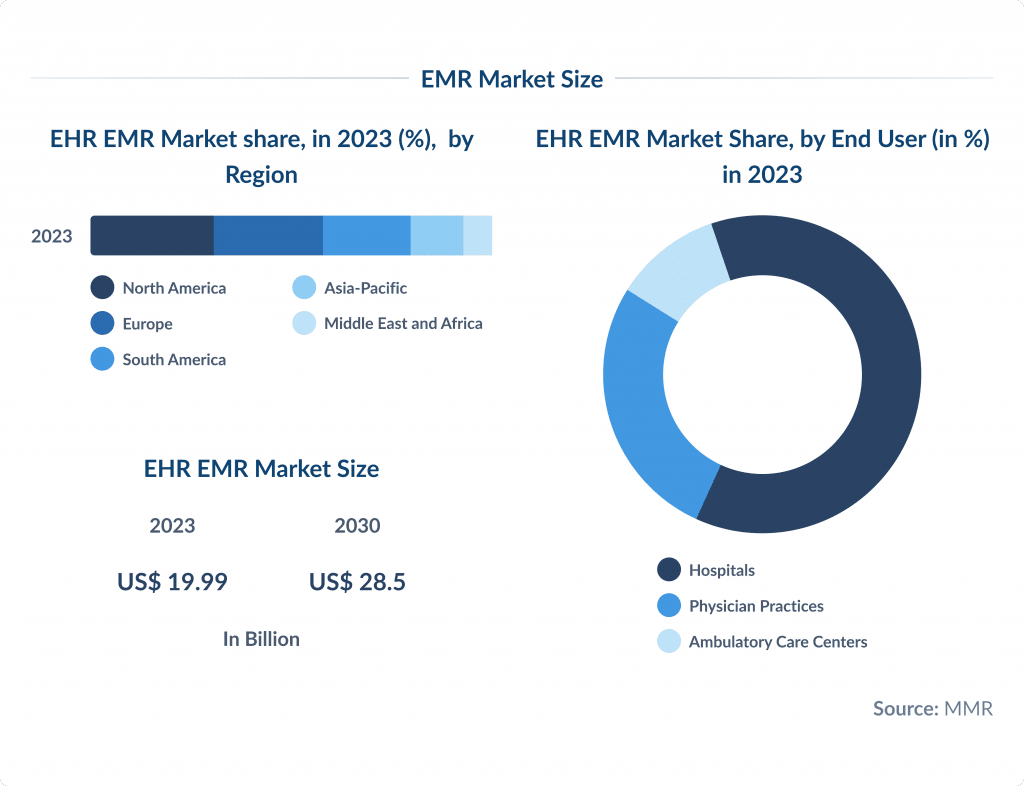
Innovation is the key to leadership. Here’s how to win the technology race in the healthcare industry.
Evolution of Medical Records: From Paper-Based to Digital Records
Medical records have existed since the beginning of medicine.
Ancient doctors used primitive tools to mark and track patient’s symptoms, treatment processes, medicine prescribed, and other important information.
When talking about modern medical records were developed in the 20th century, with data about each patient recorded, organized, and stored.
These were also paper-based at first.
However, with the advancement of technology, medical records went online.
The transition from paper-based to digital medical records has revolutionized healthcare.
Once all patient information was recorded on paper, it was difficult to access, share, and store securely within the health care organization.
With the advent of Electronic Health Records (EHR) and Electronic Medical Records (EMR), this process has become much more efficient and secure.
Discover emerging EHR startups that are setting new standards for digital health records.
Let’s compare:
Paper-Based Records:
- Patient data is handwritten and stored in physical files.
- Information is accessible only within the specific healthcare facility.
- It required a lot of space to store the data too keep it from damage and loss.
Digital Records (EHR/EMR):
- All data is entered electronically. This reduces the chances of human-made errors and saves time.
- The access to data is available across different healthcare facilities.
- Data is stored in cloud-based systems with encryption to ensure safety and security.
This evolution has improved healthcare delivery efficiency and enhanced patient care.
Suppose you are thinking about implementing an EMR solution in your organization.
In that case, you have 2 options: to select and integrate a system that is already available on the market or develop a customized solution.
Feel free to check out this guide to select the best EMR/EHR system.
In case you are considering developing your own EMR, read on as we unwrap the benefits and challenges to be aware of.
Benefits of Electronic Medical Record System Developent
If you decide to develop your own Electronic Medical Record (EMR) system, there are a number of benefits you can expect.
You can read about the benefits of EHR systems in this article.
The first benefit is customization.
Having your own system, you can add features that match your workflow and address your unique requirements. For example, you can integrate AI or AR.
This allows for a user-friendly interface that your staff or clients will find intuitive and easy to use.
Learn how AI and healthcare are shaping the future.
The second advantage is smooth integration.
With effective EHR integration strategies in mind, a custom EMR can be integrated seamlessly with existing systems and other healthcare platforms.
This elevates data sharing and communication across different departments and facilities.
The third benefit is control over your data.
With your own EMR system, you maintain full control over patient data.
Ensuring it is stored securely and managed according to your policies.
This flexibility allows you to easily update and modify the system as your practice grows and changes.
The fourth benefit is cost efficiency.
In contrast to third-party systems, developing your own system can save you money in the long term.
A custom EMR system is scalable, which means it can grow with your practice without incurring additional costs.
The cost of developing an app can vary widely. Get a clear idea of what to expect with our guide to app development costs.
Finally, a custom-built EMR system will be compliant with all the regulation and security standards you need.
You can ensure that your system meets all regulatory requirements and standards specific to your region and implement robust security measures to protect sensitive patient information from breaches and cyberattacks.
Learn about the most impactful cybersecurity trends to safeguard sensitive data and prevent breaches.
Overall, with a custom-developed EMR system, health care providers get a solution that perfectly aligns with your practice’s needs, enhances efficiency, and improves patient care. 
EMR Development Challenges & How to Overcome Them
Despite the fact that having your own electronic medical record system comes with multiple benefits, there are still some challenges healthcare providers should be aware of.
Integration with Existing Systems
Integrating new EMR systems with existing healthcare platforms can be complex.
Providers should choose interoperable systems and work with experienced IT professionals to ensure seamless data sharing and system compatibility.
Customization and Flexibility
Off-the-shelf EMR solutions may not meet all specific needs of a healthcare practice.
A customized EMR system can improve usability and effectiveness by aligning with specific workflows and requirements.
Data Security Concerns
Another significant challenge is ensuring data security and compliance with regulatory requirements.
To overcome this, healthcare providers should implement robust security measures, such as encryption and regular security audits, and stay updated on the latest regulations to ensure their EMR system remains compliant.
User adoption
It can also be a hurdle, as staff may resist changing to a new system.
To ensure a smooth transition and high user satisfaction, providers can involve staff in the development process, deliver comprehensive training, and ensure ongoing support.
Find out how long it really takes to develop an app with our comprehensive guide on how long it takes to develop an app.
Electronic Medical Record vs Electronic Health Record Systems
Despite often being used interchangeably, EHR and EMR systems have their differences. Let’s explore them further.
EMR is a patient record created by providers for specific encounters in hospitals and ambulatory environments.
Electronic health record systems are a more comprehensive collection of electronic health information for individual patients or populations.
An EHR and EMR are both digital versions of a patient’s chart.
However, EMRs cannot be shared, transferred, or accessed as easily across health care organizations.
Electronic health records (EHRs) are designed for easy sharing among everyone involved in a patient’s care, including doctors, laboratories, and specialists.
EMRs also give a narrower scope when it comes to patient data.
An EMR can give you patient demographic, diagnosis, treatment, and disease progression data.
An electronic health record contains all of the same information plus more detailed data regarding a patient’s medical history.
Overall, EHRs give a much more holistic view of a patient’s history than EMRs.
Good design can make all the difference. Check out our step-by-step guide on healthcare app design.
Step-by-Step to Develop and Implement an EMR System
There are many electronic medical record systems and electronic health records startups available on the market.
However, developing one from scratch is a great choice if your organization needs a tailored solution.
We’ve been developing electronic health record systems for over 10 years and are ready to share some insights on building and implementing a system that will cover all your needs as a healthcare provider.
Here’s a step-by-step routine to rely on.
Check Your Readiness
Before looking for an EMR system, make sure your organization is financially and operationally ready.
Ensure you have a strong business case and the right budget to implement a new system.
Consider factors like the number of patients, types of services offered, and current record-keeping methods.
You also need to identify the key features you need in an EMR system, such as patient scheduling, billing, or clinical documentation. 
Create an Implementation Plan
Now you’re ready for an EMR, plan how to build and deploy it. Your plan should include:
- Who are the key stakeholders involved in the decision making and approval process.
- A detailed timeline for each phase of the implementation, including deadlines and milestones.
- A reliable software development partner to get the development started.
- A clear communication plan to keep everyone informed of the project’s progress and changes.
- Lots of testing to find and fix any issues before go live. Check out these five usability testing ways that will help elevate your startup’s performance.
Set a Budget
Then, you need to set a realistic budget for the EMR system development and implementation.
Your budget planning should include the costs for software, hardware, training, and ongoing maintenance.
Ensure your budget aligns with your financial capacity and long-term goals.
Choose the Right Technology
Select the appropriate technology stack for your EMR system.
This includes choosing between cloud-based or on-premise solutions and deciding on the programming languages, frameworks, and databases that will support your system’s functionality and scalability.
Businesses aiming to stay competitive are investing in cloud-based app development for enhanced scalability.
Ensure Compliance
Make sure your EMR system complies with all relevant healthcare regulations and standards, such as HIPAA, in the United States.
This includes implementing robust security measures to protect patient data and ensuring data privacy.
Design and Develop the System
Work with a team of developers and designers to create a user-friendly interface.
Focus on making the system intuitive for healthcare providers and staff.
The design should include easy navigation, clear data entry forms, and quick access to patient records.
Begin the development phase by creating the core functionalities of your EMR system.
This includes patient registration, appointment scheduling, medical history recording, and billing.
Use agile development methodologies, including the agile discovery process, to build and test each feature incrementally.
Want to build a productive remote team? This guide on high-performance remote teams shows you how.
At SpdLoad, we developed DocKids, a telemedicine app that expands the boundaries of telemedicine by eliminating long queues and travel time for consultations.
Our goal was to create the easiest-to-use telemedicine application.
We started with in-depth customer research, identifying pain points like the difficulty of finding trusted doctors and the inconvenience of hospital visits.
Addressing these issues, we ensured the app allowed users to get a treatment plan in just three clicks: choose symptoms, select a doctor, and get a video consultation.
Train Your Staff
Training staff is crucial. Ensure the EMR system offers the following:
- Role-based training for different job functions.
- Strong customer support for quick and accurate responses.
- Feedback loops for continuous improvements.
Evaluate and Improve
After the system is fully implemented, continuously monitor its performance. Provide ongoing technical support to address any issues that arise. Regularly update the system to improve functionality and security.
Gather feedback from users and evaluate the system’s impact on your practice. Look at metrics like patient satisfaction, staff efficiency, and error rates. Use this information to make continuous improvements to the system.
Following these steps, we can help you develop and implement an EMR system that enhances efficiency, improves patient care, and meets the unique needs of your healthcare practice. 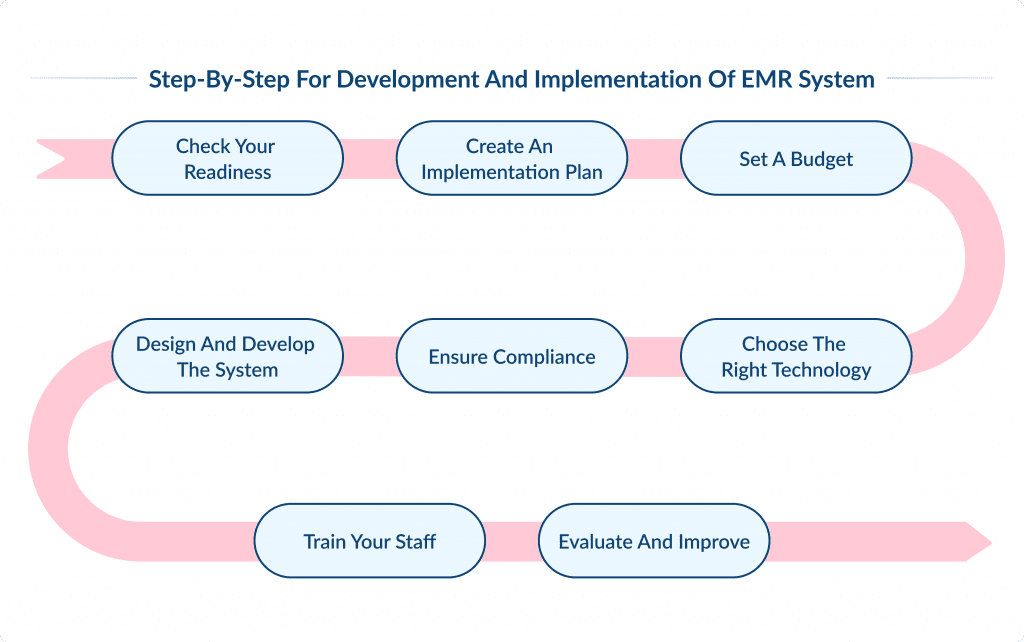
Need a reliable development team? Here’s your step-by-step guide to hiring a dedicated team in Ukraine.
Top EMR Trends for 2025
Since their invention in the 1960s, EMRs and EHRs have made tremendous progress, but there is still much to be done.
So, what the future holds for electronic health record and electronic medical health record systems?
Let’s explore.
Interoperability Policies
In 2025, EHR developers and IT specialists will continue updating systems to comply with interoperability policies.
On August 1, 2023, CMS announced a 3.1% net increase in Medicare inpatient prospective payment system rates for fiscal year 2025.
This benefits hospitals that effectively use EHR systems and maintain quality measurement data.
Additionally, CMS introduced new policies for the 2025 Medicare Promoting Interoperability Program, including a new antimicrobial use and resistance (AUR) surveillance measure.
This measure is a significant step forward in promoting healthcare interoperability.
Empower your practice with custom EHR/EMR solutions tailored just for you.
Cloud Computing
Most cloud-based EHR/EMR systems now have an interoperable architecture, enabling seamless integration with other healthcare platforms.
This integration is crucial for data sharing within the medical sector, especially for organizations looking to grow.
A Statista survey revealed that about 45% of healthcare organizations experienced phishing attacks in 2021, with 17% facing ransomware attacks and 7% reporting data breaches.
In 2022, there were 707 large-scale healthcare data breaches in the U.S., slightly down from 715 in 2021, but significantly up from 218 in 2012.
This trend has led to increased adoption of encrypted cloud computing to keep patient data secure and accessible despite cyber threats.
Standardization
EHR regulations are standardized under the Office of the National Coordinator for Health Information Technology (ONC). Practices with EHRs that don’t meet these standards face penalties and won’t qualify for meaningful use.
The ONC encourages the use of standardized application programming interfaces (APIs) to make it easier and safer for people to use smartphone applications to access structured electronic health information.
APIs integrated with EHR technology improve communication between IT systems and medical apps, enabling quick access and information exchange among multiple parties.
The guidelines stipulate that electronic access to all of a patient’s electronic health information must be free of charge.
Robotic Process Automation
Enhanced workflows and improved accuracy are driving the market for automated data capture in electronic medical records.
The global robotic process automation market is expected to grow to over $13 billion by 2030.
Robotic process automation (RPA) helps achieve the required accuracy as it eliminates the need for manual entry through.
The use of RPA allows digital labor to maintain productivity while resolving underlying issues without completely reworking the system.
Various RPA platforms integrate smoothly with existing EHR/EMR software, saving time and freeing up manual resources for essential tasks.
These integrations also help maintain compliance with data protection regulations and improve data security.
Telehealth
Integrating EHR systems with telehealth platforms helps medical organizations provide remote care and improve clinical workflows.
These integrations enable physicians to quickly and securely transfer patient information between systems.
When telehealth is combined with EMR systems, patient care in a remote environment is enhanced due to the automation of data entry, the synchronization of insurance information, the streamlining of virtual care activities, and the efficiency of collaboration between staff.
The global telehealth market is expected to grow at a CAGR of 19.7%, reaching $504.24 billion by 2030.
The growth is driven by the rising demand for EHR/EMR health apps, increased internet usage, changing population rates, and high healthcare expenditure.
IoT, AI & Voice Recognition
IoT devices are increasingly used in healthcare.
The global market expected to grow at a CAGR of 17.8% to reach $289.2 billion by 2028. Many practices are integrating artificial intelligence (AI) to help physicians diagnose and identify health trends. 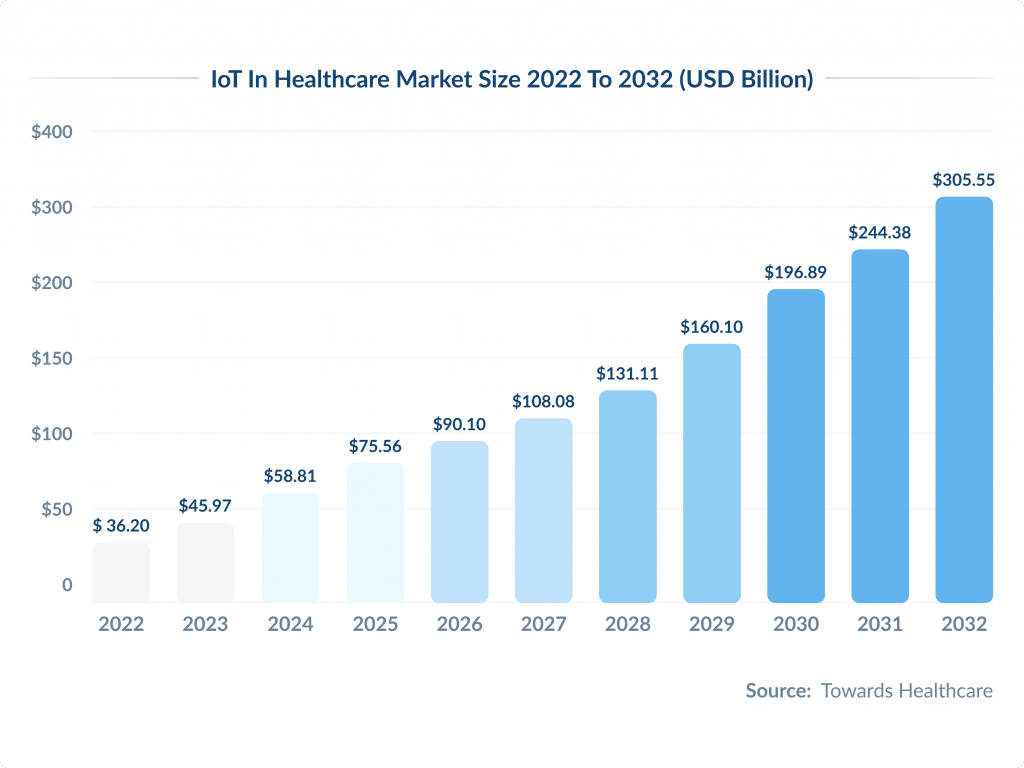
Stanford Medicine says AI can improve diagnosis and reduce administrative burden by automating data entry and scheduling.
Epic and Cerner are adding AI-driven tools to their EMR systems to streamline clinical workflows and patient care. This Cerner vs Epic guide covers more insights about these systems and how to choose one.
Some EHR’s like CareCloud Central already have voice recognition technology for data entry.
AI voice recognition can simplify documenting patient encounters as physicians can focus more on patients.
Adding natural language processing (NLP) to EMR’s can help physicians be more efficient and patient care.
AI that speaks natural language is the future, pre-authorizing insurance and giving quick input for complex cases.
With AI technology, electronic systems get faster, patient data gets analyzed quicker and healthcare professionals get help with treatment.
Let’s Move On
For anyone involved in tech, keeping up with application development trends is essential.
Electronic medical records (EMRs) and electronic health records can revolutionize healthcare.
These systems are able to improve patient care, enhance efficiency, and reduce administrative costs.
However, health care providers must recognize and address the challenges and limitations of EMRs we’ve discussed in this article.
EMRs and electronic health record systems can be fully leveraged by following best practices and choosing the right system.
At SpdLoad, we specialize in creating adaptable, HIPAA-compliant healthcare software and mobile apps that enhance efficiency and patient engagement, as well as ensure clinical data are secure.
This will prepare your practice for the future.
Ready to improve clinical workflows or make patient’s care more accessible?
Contact our experts today to discuss building the health care solutions your practice needs to thrive in the digital age.
When privacy matters, these best HIPAA-compliant chat apps are essential for secure communication.